Difference between classic IVF and IVF with ISCI
Difference between classic IVF and IVF with ISCI
Among the solutions available to the couple in the event of difficulty in procreating are IVF or in vitro fertilization. While the classic method remains widely known, the process with ISCI continues to attract attention today thanks to its high success rate. What are the actual differences between these two processes?
What is in vitro fertilization?
In vitro fertilization is one of the most common medically assisted reproduction techniques. It consists of fertilizing the oocyte in the laboratory and transferring the embryo to the uterus where it will be able to develop. This method appeared in the 1970s and has continued to evolve until today.
IVF is intended for all couples who wish to have a child, but who have a medical problem that does not allow them to procreate naturally. It may involve a genetically transmissible disease or a fertility issue involving one of the two partners.
Over the years, medicine has continued to evolve from traditional IVF to IVF with ISCI. Although both techniques produce a similar result, they are slightly different in terms of procedure.
Difference between classic IVF and ISCI
How does classic IVF work?
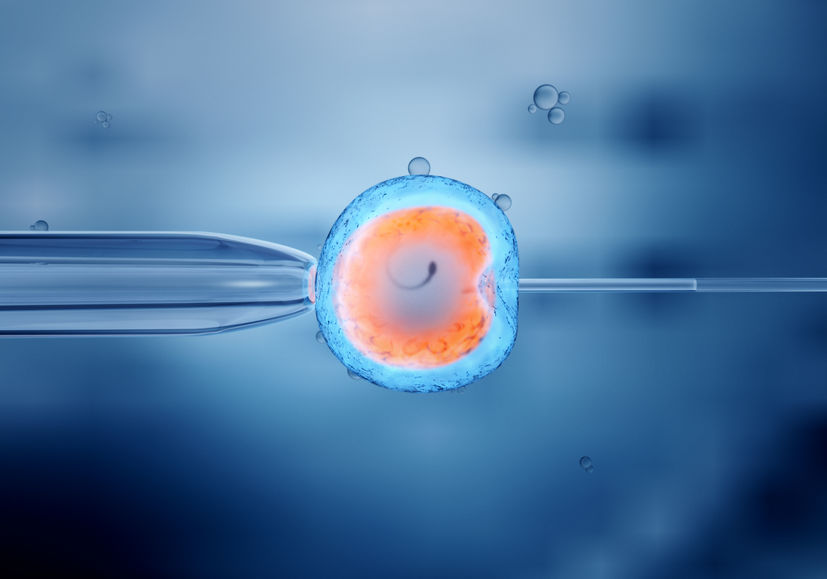
In traditional IVF, the first step is to stimulate the production of oocytes which will then be used for procreation. After the stimulation, the doctor punctures the egg with the purpose of putting it in contact with the previously collected spermatozoa.
The fertilization is performed in a thin tube where the oocyte is exposed to about a hundred thousand normal sperm. The selection is done in a natural way and only the strongest gametes manage to penetrate the outer membrane of the egg and fertilize it.
This can result in 5 to 6 fertilized eggs and, after the transfer, one of the embryos will continue to develop in the uterus. This technique has a success rate of around 24% and the number of children born from IVF was estimated at 4 million in 2012.
What is IVF with ISCI?
IVF with ISCI or Intra Cytoplasmic Sperm Injection means fertilization performed using micro-injection. This medically assisted reproduction technique was developed in 1992 in order to solve male fertility problems. It is effective in cases of oligozoospermia (insufficiency) or asthenozoospermia (poor motility).
IVF with ISCI begins with ovarian stimulation in an effort to obtain good quality oocytes. When the egg reaches its maturity, it is extracted by puncture and the egg is treated to remove its outer membranes.
Before any cultivation is made, the spermatozoa are also processed and pre-selected in order to have a greater chance of success. Each egg then receives a good quality sperm and the unused pre-embryos will be cryopreserved or vitrified. This process consists of freezing them in liquid nitrogen for later use.
What distinguishes classical IVF from ISCI?
Whether the traditional method or micro-injection is used, in vitro fertilization leads to the same result: the birth of a baby. These two techniques have many common features such as ovarian stimulation, oocyte extraction and fertilization outside the uterus.
However, the difference between these two processes lies in the execution technique. In conventional IVF, oocytes are exposed to a high number of pre-selected spermatozoa. The most resistant gametes will be able to fertilize the egg and penetrate the outer membrane. This makes the execution and success of this technique more difficult.
During ISCI IVF, the oocyte is stripped of its outer membrane beforehand and each egg receives a fertile spermatozoon. This increases the success rate and the chance of the eggs being fertilized. If this fails, the other frozen embryos can be reused.
The limitations of IVF
Like any other medical procedure, IVF has adverse effects. During ovarian stimulation, the woman may be subject to hyperstimulation, which may result in abdominal pain or swelling of the abdomen. Even if it is not severe, this symptom must be examined by a physician.
In addition, IVF may also be conditioned to the patient’s age. In fact, beyond the age of 45, the use of medically assisted procreation involves many risks. The problem can arise both during pregnancy and during the birth of the baby.
Moreover, IVF can only be performed three times in a row. If after three attempts, the patient still cannot carry the pregnancy to term, all attempts will be stopped. Nevertheless, she can still try other techniques.
In vitro fertilization also has the disadvantage of being expensive. If you have a limited budget, co-parenting may be an interesting alternative for you. If this idea interests you, consider finding the ideal partner on Coparentalys.